Welcome
Welcome to Post MD Education’s 2016-17 Annual Report. The report marks the second year in our new organizational structure which combines all medical education activities after the undergraduate medical degree. As you will see in the report, this has been a year of innovation and renewal.
Medical education is not just a program for building knowledge and skills in its recipients… it is also an experience which creates attitudes and expectations.
Through our staff, faculty and decanal leads, Post MD strives to support the medical education enterprise at the University. In partnership with our affiliated hospitals, our aim is to help faculty members, administrators, and learners achieve their goals in teaching, learning, research, clinical care, and social responsibility.
Continuing Professional Development’s excellent support allows our departments to offer accredited, outcome-based continuing education conferences and programs. CPD activities reach over 40,000 learners annually through its in-person and on-line events, including its award-winning Safer Opioid Prescribing multi-modal program. CPD also promotes cultural competence and health care provider networking through development and promotion of the bi-annual North American Refugee and Indigenous Health conferences. Associate Dean Suzan Schneeweiss also launched an ambitious five-year plan to renew CPD’s academic mission under four priority areas: Leadership, Innovation, Scholarship, and Community.
Under the leadership of Associate Dean Glen Bandiera, postgraduate medical education activities included the dissemination of Best Practices in Assessment and Evaluation and on-line system development, a transitions forum, Global Health programming and conference, the creation of the Postgraduate Administrators Advisory Committee, expansion of the learner experience survey (Voice of the Resident), and faculty development workshops for the implementation of competency-based medical education (CBME). On CBME, you will no doubt enjoy the videos of the two early adopters of the new training structure (Drs. Paola Campisi and Scott Berry) as they outline their “lessons learned”!
Other Post MD innovations include the creation of the Simulation Education Advisory Committee, chaired by Dr. Douglas Campbell which brings together the Faculty’s simulation experts and resources. In addition, a new grant to support Medical Humanities Education and an award to recognize contributions to social justice and health equity in faculty development were established.
I hope this report reflects Post MD’s ongoing commitment not only to excellent medical education, but as Flexner notes, to create in our faculty and learners “…attitudes and expectations” based on a core set of values and the desire to achieve them.
Salvatore M. Spadafora MD FRCPC MHPE
Vice Dean, Post MD Education
December 2017


Strategic Plan Integration across the continuum
Within the new Post MD Education structure there are opportunities for integration and alignment which will enhance the ability to harness more talent and increase influence across sectors. Post MD Education is working to address this through strategic planning at Postgraduate Medical Education (PGME) and Continuing Professional Development (CPD).
As PGME starts the strategic planning process, addressing the significant changes in the external environment will be a priority. This includes but is not limited to: the conversion to CBME, new accreditation standards, new accreditation processes, CanMEDS 2015, and increased accountability requirements for funding and health care provision. In keeping with the University of Toronto Faculty of Medicine Strategic Plan, the objective for the five year PGME strategic plan will be to enable and support partners and programs that establish, meet and exceed best practices in the education of physicians as emerging leaders.
For CPD, the strategic planning process has recently been completed. Over the past year, dedicated working groups representing a number of stakeholders were engaged to develop a flexible and adaptable 5-year strategy. The groups synthesized ideas from the CPD Strategic retreat to develop goals, objectives and action plans that renewed CPD’s academic focus and established the path for the next five years. In the next 6 – 12 months CPD will focus on building capacity in research and scholarship, maintaining its leadership role in continuing education with the development of internationally recognized programs and exploring technology platforms for self-directed learning. CPD will also strengthen partnerships with internal and external organizations to integrate quality improvement in its offerings.

Competency Based Medical Education A learner centred and outcomes based framework
CBME is an outcomes-based approach to medical education, which uses competencies as the organizing framework. Thus by definition, CBME demands new attention to assessment techniques (Holmboe, 2010). Challenging older norms, which prioritize learning methods of “steeping” or repeated exposure, CBME is understood to “de-emphasize time-based training and promise greater accountability; flexibility, and learner-centredness” (Frank, 2010). This framework for learning has been adopted by PGME and CPD at Post MD Education.
The postgraduate medical education landscape is actively changing and is in the early stages of implementing CBME in Canada. As these changes are being implemented across post graduate programs, it is important to focus on the development of best practices in resident evaluation and assessment that can support its adoption. To this end, the Best Practices in Evaluation & Assessment (BPEA) Working Group was established in 2016 to help inform PGME in best practices for resident evaluations and assessments. The group conducted literature reviews and focus groups with residents and faculty leaders and prepared several papers on various aspects of assessment including faculty and resident responsibilities, remediation, data management, and learner handover.
The top 5 priorities identified by the Working Group are:
- Faculty development resources (e.g. central shared repository and best practices for assessment)
- Shared repository of education and assessment tools for individual programs
- Centrally organized and supported IT for CBME, including support for reporting and data extraction
- Mobile, lightweight, flexible, easy-to-use IT
- Learner responsibility for their education, including adjustments to new assessment systems
The full BPEA report is available on the Post MD website at http://cbme.postmd.utoronto.ca/BPEA/
CPD is also participating in this new era of Canadian medical education by adopting a CBME framework. For an office that delivers approximately 400 continuing education programs each year, the shift means integrating new methods of assessment and evaluation of participants’ learning needs and the extent to which these are met. CPD’s activities and programs have been aligned to promote the core competencies identified by the Royal College’s Competency by Design (CBD) and the CFPC’s Triple C Competency Based Curriculum.
In June 2016, CPD implemented CFPC’s newly launched Mainpro+ credit system, which introduced new criteria to track physician competencies. As part of the implementation, the CPD Accreditation team revised the accreditation application form to meet the new standards outlined by the CFPC. Educational sessions were held with the CPD D&L committee in June 2016 and also with Departmental CPD administrators in September 2016 to ensure that faculty and staff were aware of the changes.
The CPD Accreditation team continues to encourage pre-and post-assessment activities which provide opportunities for self-directed learning. Demand for accredited courses that use multi-faceted methods of learning and assessment, such as ImageSim, continue to grow. It is clear that discernible efforts towards integrating principles and building a new culture of competency-based education and assessment are underway at CPD.

Scholarship at PostMD Furthering Research and Celebrating Excellence
The research and scholarship mission of Post MD Education continues to be furthered by the papers, posters and workshops facilitated at local, national and international conferences. In 2016 and 2017, 10 papers, 24 workshops, and 4 posters were produced through the PGME office. CPD related scholarship across the Faculty of Medicine included 161 papers, 45 presentations at CCME, 7 grants. In addition to this, Post MD is responsible for the adjudication and administration of 17 teaching and research awards and grant programs. These awards and grants celebrate excellence and further research across the continuum. View the complete list of the awards and grant program criteria and recent winners.
To further support scholarship activities, a new award, a new grant, and additional staff were added to the portfolio.
The Dr. Robert H. Sheppard Award for Health Equity and Social Justice was established in 2016 to acknowledge the humanitarian work of the late Dr. Robert H. Sheppard, former dean of postgraduate medicine 1977-1988. The award recognizes outstanding contributions of faculty members and medical trainees involved in activities, programs or research related to social justice and health equity in faculty development or postgraduate medical education.
In January 2017, Post MD Education initiated a grant to support projects in Medical Humanities Education. The grants will support projects that enhance humanism, compassionate care, clinical competencies and deliverables. These areas are closely aligned with the ongoing priorities of postgraduate medical education and the CanMEDS roles. There will be a call for proposals and awarding of the grant on a semi-annual basis.
Dr. Walter Tavares was appointed to the role of Scientist and Assistant Professor at the University of Toronto / University Health Network Wilson Centre in Post MD Education in the Faculty of Medicine on September 1, 2016. Dr. Tavares obtained his PhD at McMaster University in Clinical Epidemiology and Biostatistics while completing a 5-year masters and PhD fellowship at the Wilson Centre. His research examines ways of optimizing performance based assessments in work and simulation settings.
Dr. Paula Rowland was appointed to the role of Scientist and Assistant Professor at the University of Toronto/University Health Network Wilson Centre in Post MD Education in the Faculty of Medicine on October 2, 2017. Dr. Rowland previously held positions with the University Health Network’s Collaborative Academic Practice Portfolio and the University of Toronto’s Centre for Interprofessional Education. Dr. Rowland holds an appointment in the Faculty of Medicine, Department of Occupational Science and Occupational Therapy as well as the Rehabilitation Sciences Institute at the University of Toronto. Her research explores questions of professional practice, attending to the intersections of organizational contexts with the ways in which we learn and work.
Dr. Tavares and Dr. Rowland’s responsibilities include leading high quality independent research programs relevant to Post MD Education and mentoring, collaborating with, and consulting with other education scientists, education researchers, clinician investigators and graduate students in healthcare education projects.
In addition to these appointments CPD has also recruited Shiphra Ginsburg, MD, MEd, PhD as Academic Director and Morag Paton, MEd as Education Research Coordinator.
Dr. Ginsburg is a Professor in the Department of Medicine and a Scientist at the Wilson Centre for Research in Education. She joined CPD in July 2017. Her program of research involves two inter-related areas. The first explores how clinical supervisors conceptualize, assess and communicate about the performance and competence of their learners, with a focus on the language used in workplace-based assessment. The second area explores the construct of professionalism in medical education, from the perspective of learners, faculty and practicing physicians. Ms. Paton joined CPD in May 2017 from previous roles in the Office of the Education Vice-Deans and the Department of Family & Community Medicine. She is a flex-time PhD student in Higher Education at OISE. Together this group will work to build capacity on education scholarship across CPD, including providing scholarly consultations for faculty and staff. Under the new CPD Strategy, this team is currently engaged in an environmental scan of CPD scholarship across the Faculty, and is reaching out to the CPD community to identify opportunities and best practices in this area.

Transitions – From MD to Residency to Practicing Physician
On Friday, April 7, 2017, the Faculty of Medicine hosted a “Transitions Think Tank” with approximately 40 participants. The forum brought together learners and faculty from the MD program, Postgraduate Medical Education and Continuing Professional Development sectors to have honest conversations and share ideas about transitions within medical education, with consideration of ongoing activities at the provincial and national level.
The event was designed to:
- Discuss key issues related to transitions across the medical education spectrum.
- Reconcile different perspectives about key transition points along the spectrum.
- Distinguish local, provincial and national opportunities to improve transitions
- Identify ideas and recommendations about how U of T can lead innovation in transitions.
Long-standing concerns were discussed including the CaRMS selection process, true residency program requirements, medical school academic records, alternative careers, timing of residency program choices and system inflexibility, the importance of research, and readiness for practice. Possible action items emanating from the forum were a plan to standardize UG learner reports, limitations on elective rotations, improved health workforce data, and clarity from programs on the need for research experience. For more information on the discussion points of the forum, please download the PDF.

Indigenous and Global Health Expanding Education Opportunities
Indigenous and Global Health are two important areas within PostMD Education. Through CPD, the Indigenous Health and North American Refugee Health conferences explore issues and discuss solutions to address the needs of these populations. At PGME, Global Health (GH) is a department which develops and delivers coordinated, inter-specialty education and programming with a view to improving health in Canada and abroad. GH has a number of initiatives that reflect PGME’s commitment to local and global social responsibility and accountability. CPD has been working towards increasing cultural competency through several initiatives led by Dr. Anna Banerji the Faculty Lead for Indigenous and Refugee Health with Post MD Education.
Through Global Health electives, residents and fellows can gain an understanding of varied health systems and social determinants of health. For those interested in more intensive global health education, the Global Health Education Initiative (GHEI), now in its 9th year, is a two year, 25 module certificate program. Over 100+ participants, 100+ faculty, and 200+ graduates are part of a strong GHEI alumni network.
Celebrating the accomplishments of GHEI graduates and showcasing leaders within the global health field, PGME’s annual Global Health Day is dedicated to urgent global health issues and themes. In addition, regular educational and experiential opportunities such as alumni workshops lectures and seminars, journal clubs, and research day also support continuing education, teaching and professional networking in this area.
CPD’s Indigenous Health Conference was launched in 2014, the biennial conference takes the unique approach of sharing the distinct health needs of Indigenous peoples through Indigenous voices. This population continues to experience significant health disparities on every major health indicator and are underserviced for quality healthcare.
Dr. Anna Banerji, conference co-director, sees it as a way to create a space for Indigenous voices to state what is needed for their communities and for health care providers to become advocates. “So many historical and contemporary issues have had a devastating impact on the health and well-being of Indigenous populations.” She believes continued dialogue with Indigenous peoples, health experts, policy makers and health care providers are key to improve health outcomes.
Another initiative lead by Dr. Banerji through CPD is the North American Refugee Health Conference (NARHC). NARHC is the largest refugee health conference of its kind and was recently held in Toronto. Designed for those at the frontline in addressing refugee health needs, this biennial conference welcomed over 650 speakers and participants in 2017.
As interest in global, refugee and Indigenous health continues to grow, the programming offered by both PGME and CPD will continue to meet the need for education in these important areas.
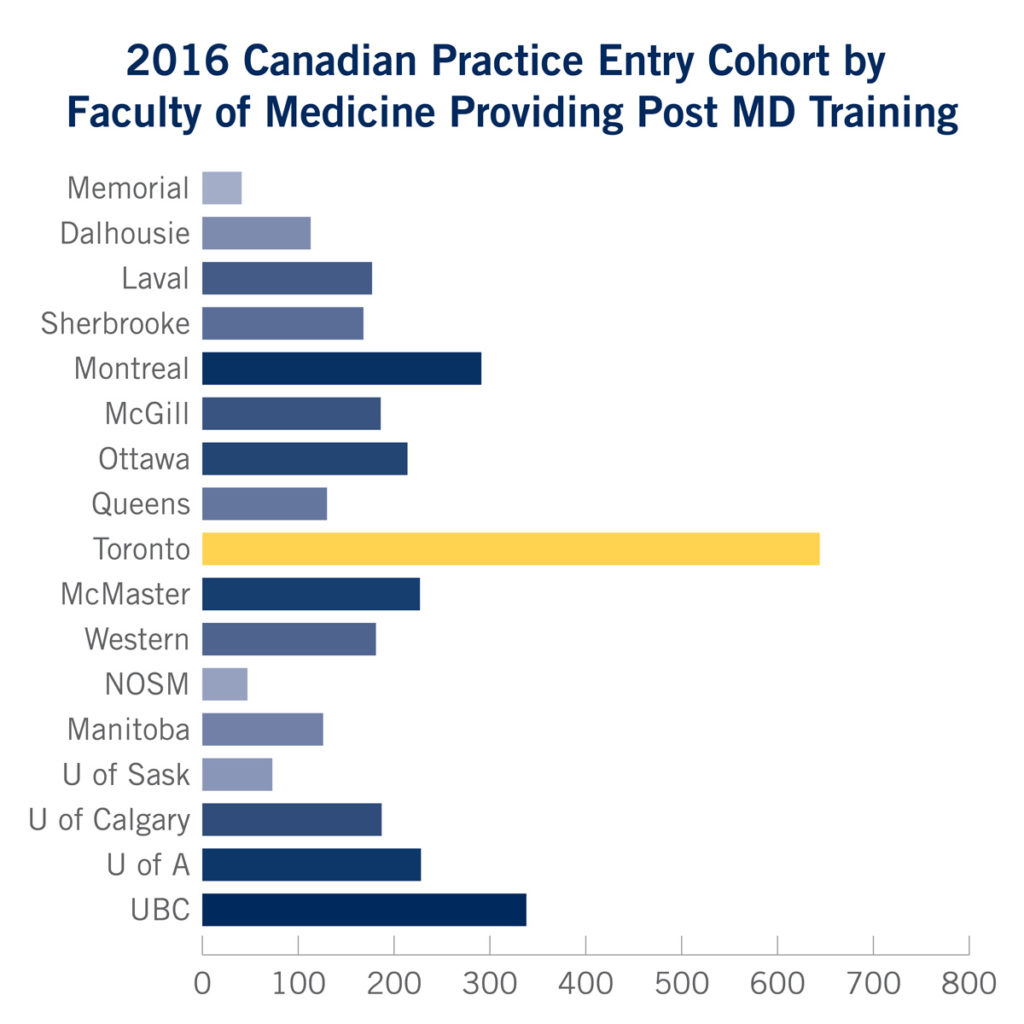
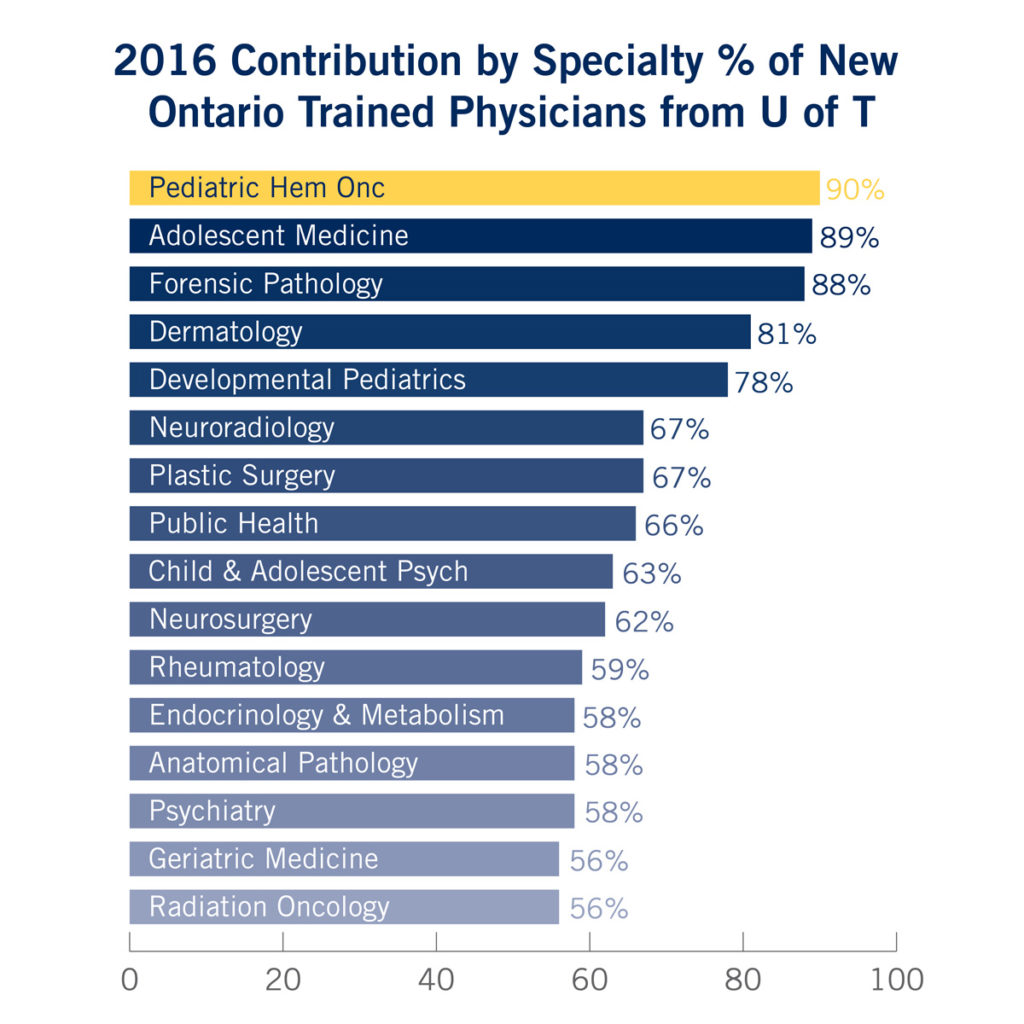
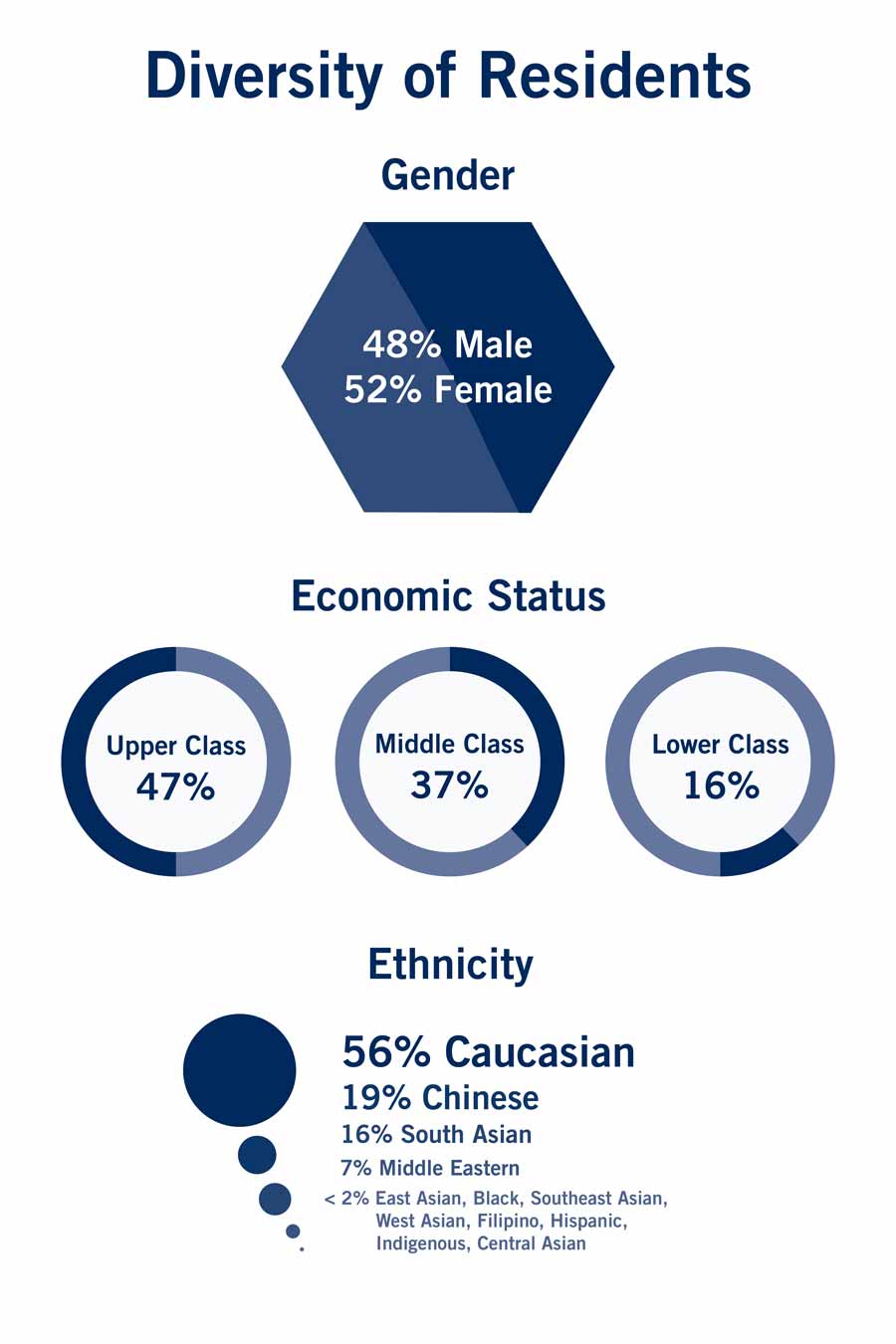
Learner Statistics Across the Continuum
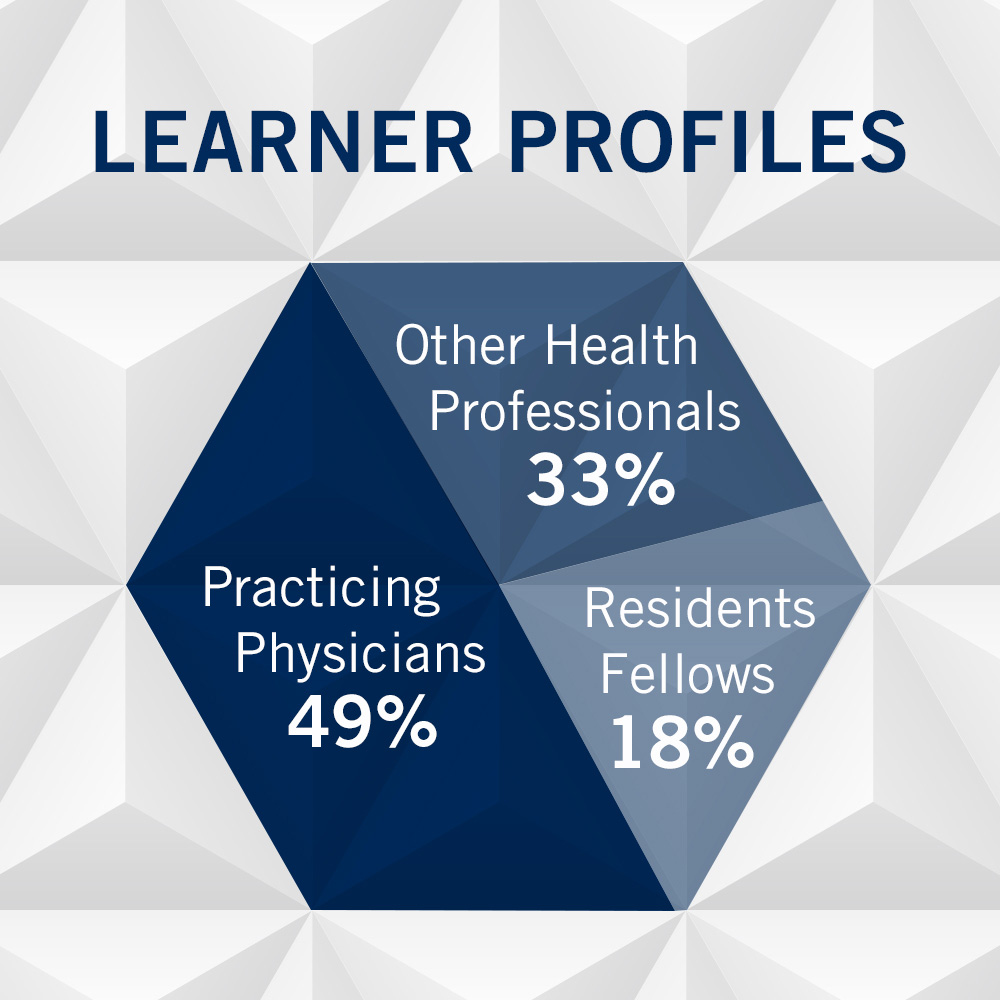
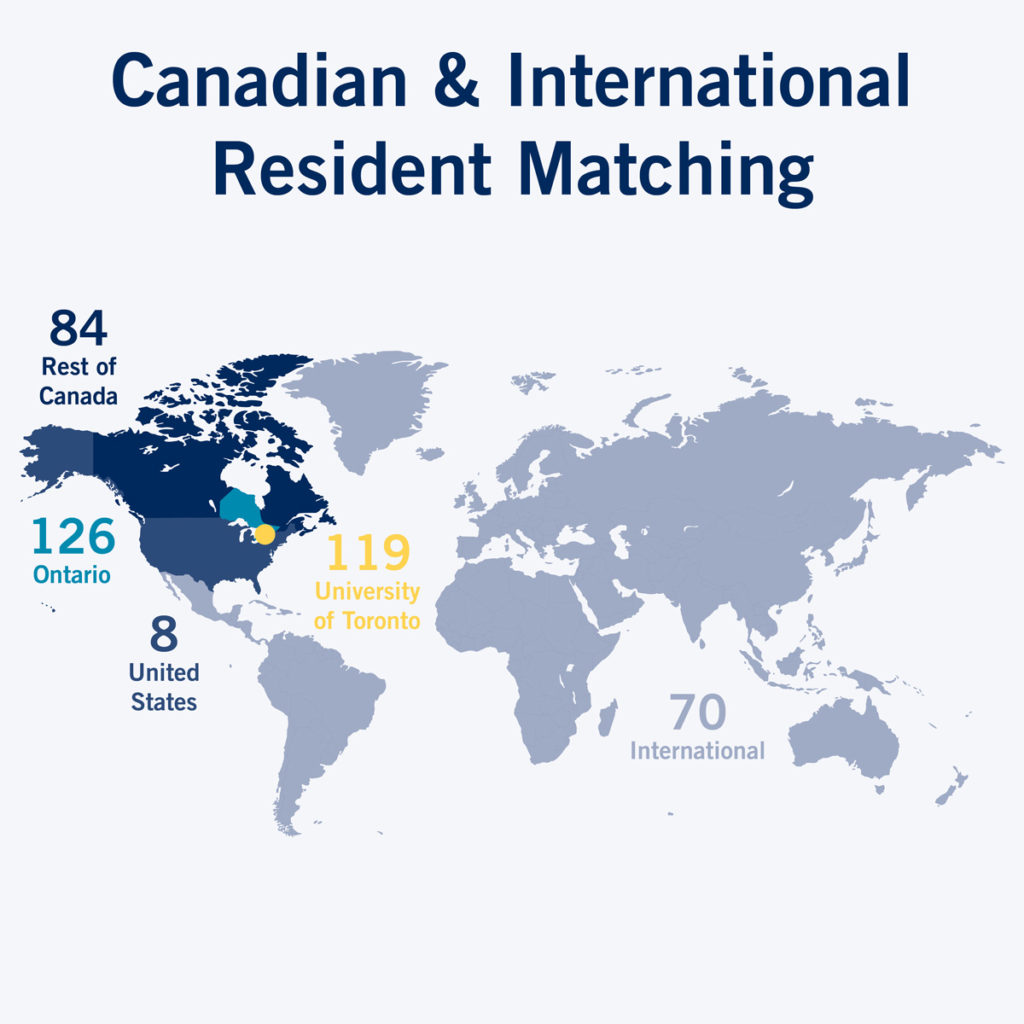
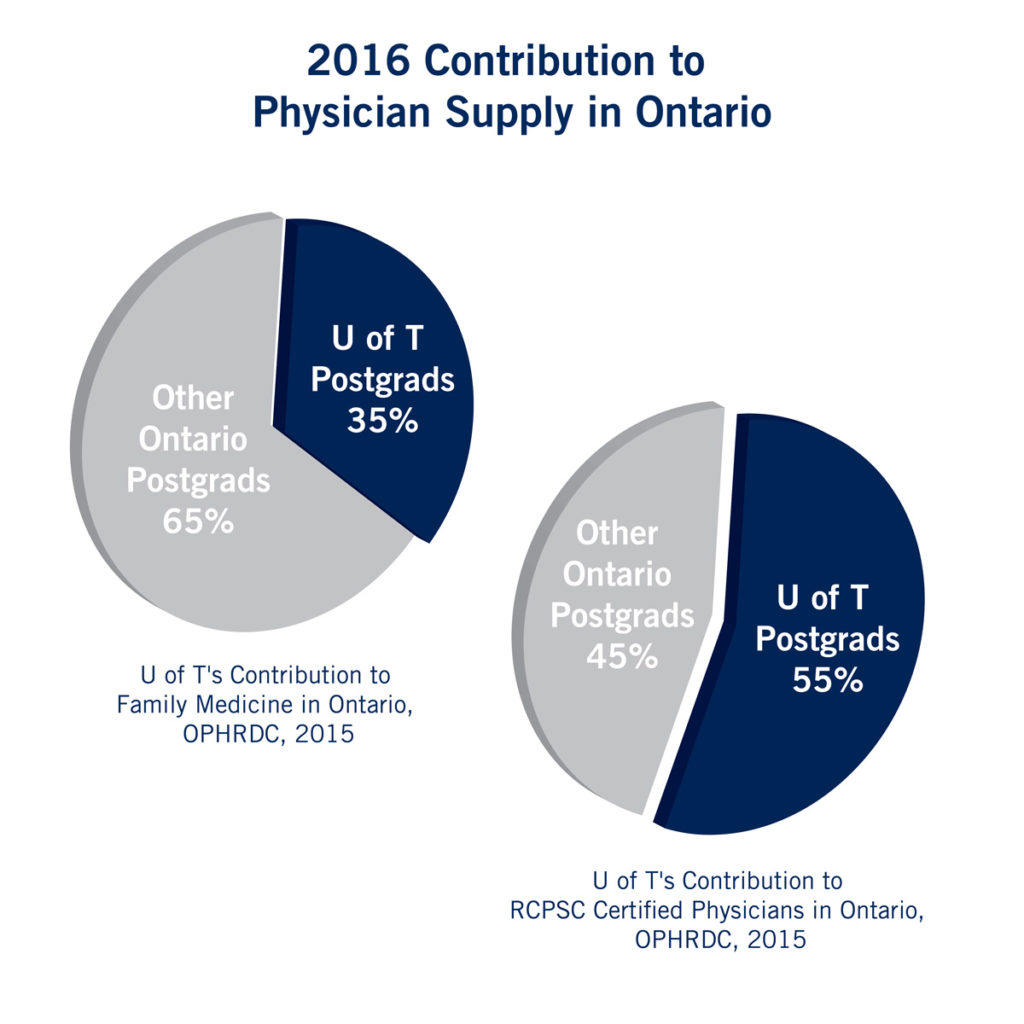
Programs, courses, conferences and events offered by PGME and CPD focus on all medical education after the undergraduate medical degree. Statistics from 2016 and 2017 provide insight into types and number of activities, the profiles of the learners including their specialties and the contribution of these learners to the physician supply.