Welcome to the 2017-18 Annual Report for Post MD Education, outlining some of the achievements and progress in the goal of Postgraduate Medical Education (PGME) and Continuing Professional Development (CPD) to provide excellent programs and support to our learners, faculty, administrators, practicing physicians, and hospital partners.
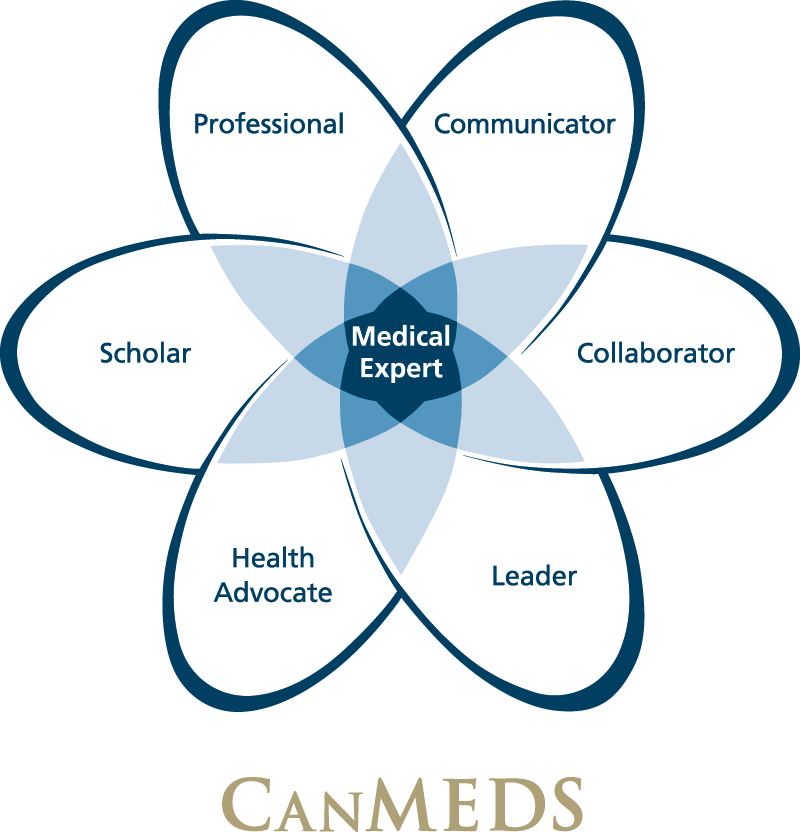
With the focus of this past year on Competency Based Medical Education (CBME), it is no surprise that the theme of this year’s report is “Competencies”.
For postgraduate medical education, CBME is an opportunity for enhanced tracking of resident progress and a positive change in the feedback process. You will read about the experience of Anesthesia and Otolaryngology-Head and Neck Surgery — the first programs to undertake this cultural shift in assessment of medical education. With appropriate faculty/resident development and program evaluation, future cohorts transitioning into this new model will benefit from these early adopters.
The competency based rubric has also changed program offerings and curriculum in CPD. The “Leading and Influencing Change in CPD” program restructured under Associate Dean Suzan Schneeweiss now offers more learner-centred instruction and coaching to assist in participant development.
CPD underwent a very successful external accreditation review in March 2018. The review noted strong decanal support, a creative mix of programs, research, and professional services model. In preparation for PGME’s formal accreditation survey in Fall 2020, our residency programs are engaged in a self-study process to prepare for assessment according to new RCPSC accreditation standards, and a mock review of the PGME office is scheduled for November 2018.

In the Research and Awards section, the report places a well-deserved spotlight on the retiring Dr. Ivan Silver who has served the Faculty of Medicine in a variety of roles during his tenure, an innovative proponent of scholarship, continuing education, inter-professional development and collaboration. Also highlighted is a program which received the Royal College CPD Providers Innovation Award, the Certificate Program in Foundations of CPD, which provides training in the development of effective CPD activities.
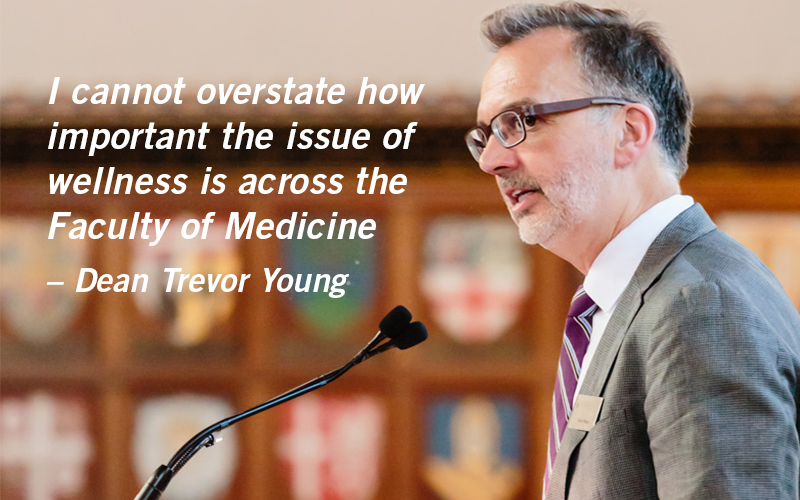
Our efforts to create a sustainable culture of wellness continued this year with CPD’s workshop on Wellness for Healthcare Professionals, offered as part of the U of T Alumni activities. The increased use of the Office of Resident Wellness is reflective of this ongoing challenge, and the Office has organized sessions at learner academic half-days to discuss the impact of clinical work on mental and physical health.
Along with changes in modes of program delivery, CPD implemented a more stream-lined system for faculty applying for accreditation of their workshops/conferences. PGME system development is highlighted under Elentra, an assessment platform enabling workplace assessment for residents in a clinical setting. The platform was successfully piloted in 2017-18 in collaboration with Discovery Commons using real-time, point of care assessment tools. Further developments will be made in conjunction with CBME programming.
The report also features a number of innovations at Post MD Education this year such as the simulation symposium held in January 2018 at Hart House, where innovators in the U of T community presented on their cutting-edge technology within the simulation sphere. In addition, PGME expanded its leadership program from the single annual workshop in August for chief residents to a series of reception-style networking events with keynote speakers.
In closing, I would like to acknowledge the ongoing commitment and dedication of Associate Deans Dr. Suzan Schneeweiss and Dr. Glen Bandiera and the extraordinary efforts of staff and faculty in our community. I am proud of all we have been able to accomplish together.
Salvatore M. Spadafora MD FRCPC MHPE
Vice Dean, Post MD Education